Andrew C. Cobb, DDS
Author’s Note: This article provides the rationale and importance of mounted models as an integral part of the records process. It also provides information to help avoid some of the more common problems associated with fabricating mounted models and is not intended to be a step-by-step guide. For procedural or stepwise information, please see the educational resources at www.thedawsonacademy.com.
The foundation for complete dentistry is based upon the execution of a complete and thorough examination. The examination includes the evaluation of the entire gnathostomatic system, including the temporomandibular joints, muscles of mastication, teeth, and supporting structures. The system is checked for signs of instability, which may be rooted in microorganism-induced breakdown (caries and periodontal disease) or functionally trauma-induced breakdown (occlusal disease). The ability to thoroughly examine the system for signs of instability is paramount to establishing a comprehensive treatment plan that takes into consideration the causes of deterioration and possible solutions.1
Essential is a records-gathering process for the evaluation of the gnathologic system, a means to evaluate the temporomanbibular joints, a digital camera, and a semiadjustable articulator that accepts a face-bow transfer. Each is equally important to the successful creation of a thorough comprehensive treatment plan that assures patients long-term stability through elimination of both pathologically and functionally induced problems.2 In addition, esthetic needs and wants of the patients are addressed.
Face-Bow Mounted, Centric Relation Articulated Mounted Models
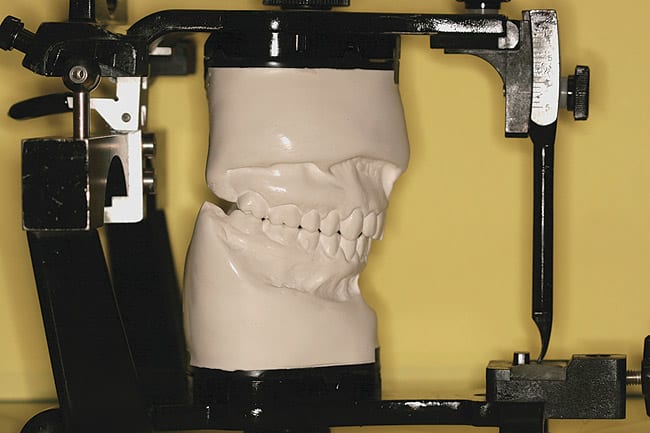
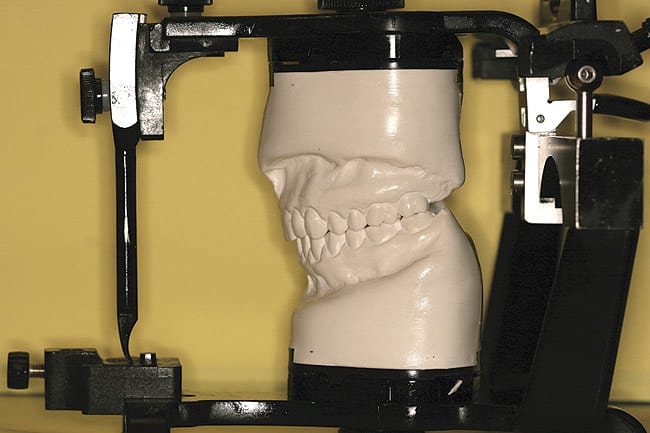
Accurate diagnostic models mounted on a semiadjustable articulator, using a face-bow transfer in centric relation, are key to the success of any thorough evaluation and treatment plan. Essentially, this provides a way for the dentist to study how the patient’s mandible and its dentition relates to the maxilla and its dentition in centric relation (Figure 1 ). Meticulous attention and the establishment of an in-office protocol are required to assure accuracy. Dentist and staff, with everyone having a clearly defined role, must share in this process. Ideally, once a protocol has been established, a trained laboratory assistant performs much of this process. Failure in any step is magnified and compromises the diagnostic and restorative outcomes. It is unfortunate if the treatment is based on an inaccurate set of mounted diagnostic models or a pretreatment diagnostic wax-up has the incorrect occlusal scheme. It is worse if the restorative try-in of a prosthetic case does not fit due to inaccuracies from the office’s records process.
The author’s father, Dr. Everett Cobb, taught both dental materials and operative dentistry courses at Georgetown University’s dental school. He would repeatedly challenge his students with this question: “What is the most important step to any procedure?” The answer: “The one you’re on.” Nowhere in the records process is this truer than in the creation of face-bow mounted, centric relation-articulated diagnostic models. Attention to detail will help assure success.
The process involves six key steps to assure accuracy:
- Diagnostic impressions
- Materials
- Face-bow
- Centric relation record
- Mounting the models
- Articulator settings—condylar path
Diagnostic Impressions and Models
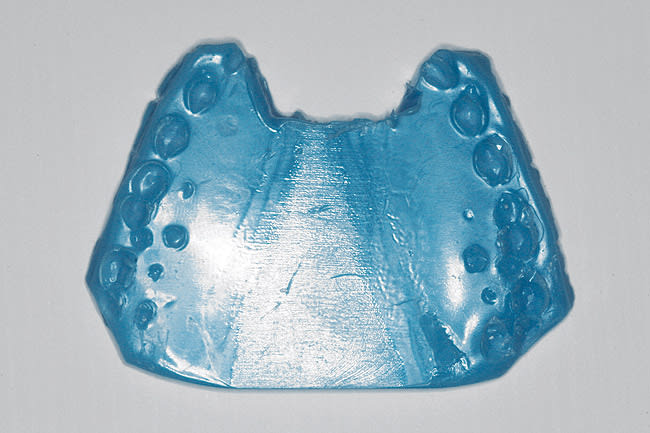
Essentially, the diagnostic models need to be a re-creation of the patient’s maxillary and mandibular arches, with an accurate representation of the teeth and supporting tissues. This starts with precise impressions that capture these structures. The impressions should include the teeth, gingiva, palate (on the maxillary impression), frenum, and extension of the impression into the vestibule. The teeth should be free from voids and occlusal artifacts (Figure 2). Such artifacts could result in an unstable fit to a face-bow or centric relation record, leading to a mismounted model. The gingival tissues need to be well reproduced, especially because macro- and microesthetic decisions pertaining to smile design may be partially based on the models. An “unreadable” model will render these decisions difficult.
The supporting structures such as frenum attachments, palate, and alveolar process also need to be recorded. A “U-shaped” maxillary impression without the palate is not accurate. The supporting structures are needed for proper evaluation and possible stabilization of guides and stents to be used in the restorative phase. Envision a case in which most of the maxillary anterior teeth are to be prepared and accurate provisional restorations based on a pretreatment wax-up stent is to be used. The palate is needed as a stop to the provisional stent. Without it, the provisional stent cannot be properly seated, leading to inaccurate provisional restorations.
Materials
Dental materials is one of the first courses taught in dental school. Often, dentists may not spend adequate time to stay informed of the recent developments in this ever evolving area. Many of the most important advancements in dentistry would not have occurred if not for the improvements in materials. Some of these newer materials can help improve the accuracy of impressions and models.
For years, dentists have used one material to create study models and another, more accurate impression material for final crown-and-bridge working models. If the goal is accuracy, why would dentists not want to use a more accurate material? The more closely a patient’s dentitions can be reproduced, the more precise dentistry will be.
For years, irreversible hydrocolloids (alginate) have been the standard impression material for creating diagnostic models. When used correctly, it can create a very accurate impression. However, by today’s standards and by dental professionals’ requirement for the most accurate impression possible, alginate has some disadvantages. Alginate is not dimensionally accurate for the long term and can distort within minutes. It is affected by humidity and temperature and can be poured only once. In addition, alginate is affected by some surface disinfectants and is subject to inaccuracies in water-to-powder ratios and mixing techniques.3
Alternatives to irreversible hydrocolloids include polyvinyl siloxanes (PVS), which improve upon many of alginate’s shortcomings. It is dimensionally more accurate and stable and can be sent to a laboratory. It can be poured multiple times and is not affected by surface disinfectants. Disadvantages include a slightly longer set time, which can be an issue for some patients (Figure 2).
In reality, both materials are needed. Most preliminary impressions can be taken with PVS for the improved accuracy. When alginate is used, dentists can try to limit the variables as much possible. Precisely following the manufacturer’s instructions for water-to-powder ratios, using an auto mixer for thorough mixing, and pouring the model immediately after the impression is taken all will improve the accuracy of an alginate impression.
Once the impression is perfected, a model should be based on that impression. Attention to detail and following the manufacturer’s directions for the material is essential. When comparing dental stones commonly used for models, a less accurate stone, with a greater degree of dimensional instability, is often the choice for diagnostic models and a more precise stone, with less dimensional change, for working models. Why would dentists want to be inaccurate with diagnostic models from the very beginning? The closer the models represent patients, the more accurate diagnostic and clinical treatments will be.
To create the most accurate model, dentists want to use the most accurate materials and to standardize techniques. Generally speaking, die stone is one of the most accurate stones and generally has a thermal expansion percentage of less than 0.10%. In creating the most accurate model, a stone with a degree of thermal expansion closer to die stone is used. Many options are available and easily identified once dentists take time to investigate. Orthodontic stone tends to be more accurate and can be found with an expansion of less than 0.10%. The stone also has to be mixed per the manufacturer’s instructions, which includes proper water-to-powder ratios (that is, weighing the stone and measuring the water). Standardizations can be created in the office to simplify this step. In addition, a vacuum mixer is invaluable for helping eliminate air bubbles.
To create a set of models that most relate to patients, dentists need to start with the most accurate materials for both impression and dental stones (Figure 3). Manufacturers’ protocols need to be followed. Abbreviating steps will result in bigger problems. Properly trained staff members are essential to this process and often may perform the task better than the dentist.
Face-bow
The face-bow is essential for establishing the incisal/occlusal plane of the maxilla and recording the condylar axis. Thus the proper arch of closure is recorded and relates the maxillary model to the articulator mirroring the same relationship as is in patients’ skulls.4 Face-bow mounting of the maxillary model is the first step in the mounting process.
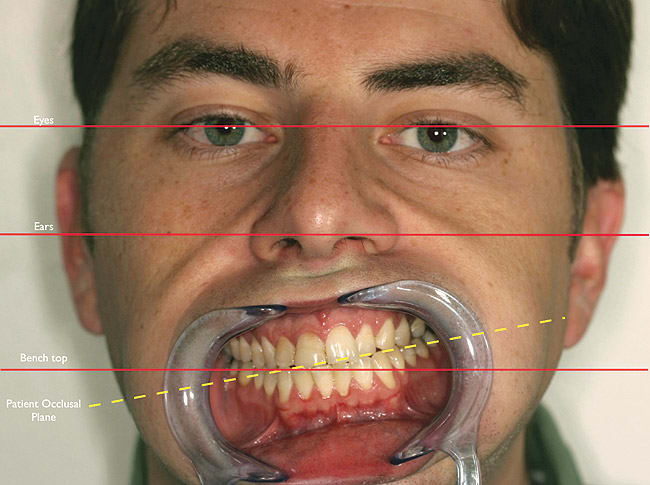
Many types of face-bows are available and relate to the various articulators. One of the most common is an earbow, which uses the ear as a reference point. With the patient upright, the bow of the face-bow is related to the ears and eyes. In most circumstances, the bow is parallel to the eyes, ensuring that the mounted maxillary model has an occlusal plane aligned with the bench top. This allows the dental technician to create anterior restorations with an accurate incisal plane and proper central incisor embrasure. Inaccuracies in the face-bow can lead to a mounting that is set at an angle, which, in the case of anterior restorations, can lead to the creation of a cant or occlusal plane discrepancies.
Under most circumstances, the interpupillary line is correct, however, sometimes, both the ears and eyes may have discrepancies. In such cases, a simple level attached to the bow may aid in establishing the proper incisal plane (Figure 4). This step is critical when anterior restorations are planned. In addition, the face-bow photograph is a valuable laboratory communication tool when facial discrepancies are apparent (Figure 5).
Centric Relation Records
Much has been written about occlusal bite records and methods for obtaining accurate and repeatable centric relation bite records. A study by McKee showed obtaining centric relation records was learnable and repeatable.5 One of the main purposes of the mounted models is to evaluate the relationship of the mandible to the maxilla. In addition, by establishing the proper arch of closure, changes to the vertical dimension while maintaining centric relation can be evaluated.6
Similar to McKee’s study, the method for obtaining a centric relation bite record taught by Dawson and the Dawson Academy has shown obtaining an accurate and repeatable centric relation record is teachable and repeatable. Following this bilateral manipulation technique using Delar wax (Delar Corp, Portland, OR) a centric relation bite registration can be obtained and used in the mounting process. Discrepancies that occur when mounting the mandibular model with the centric relation record are often caused by a human error. Accuracy of the dental practitioner’s models again is paramount to proper mounting. If the occlusal surface of either model is not precise, the model will not properly relate to either the face-bow transfer or centric relation record. Accuracy of models and techniques simplifies this step. In addition, if the bite registration material is more accurate than the models, it will not properly fit. Both of these discrepancies will lead to an inaccurate mounting of the models. The ideal bite registration using Delar wax as the registration material has cuspal indentations but not the entire occlusal surface and secondary anatomy. The recording of just the cusp tips will ensure that the records will precisely fit the models and allow for accurate mounting of the diagnostic casts (Figure 6).
Mounting the Models
Once the models are poured and trimmed and the face-bow and centric record obtained, the models are mounted. The maxillary model is mounted first via the face-bow and mandibular model and then mounted to the maxillary model via the centric relation record. One of the keys to creating the proper mounting is to verify that the models fit the face-bow and centric relation records perfectly without any rocking or imperfections. If the models do not fit, imperfections on the occlusal surfaces of the models or a bite record that is too accurate is most likely the cause. A second possible cause of incomplete seating is a bite record that impinges on the soft tissue. In this case, the tissue-bearing area needs to be relieved to allow seating.
Mounting stone is also critical for accuracy. If the stone has a high degree of thermal expansion or the dentist uses an improper technique for measuring or mixing the stone, the mount will be incorrect. Mounting plasters tend to have a high percentage expansion and are generally not the best choice. The ideal mounting stone should have a low percentage of expansion similar to the model stone and also be less than 0.10%. Proper water-to-powder ratio is also necessary for accuracy.
Articulator Settings—Condylar Path
There are some norms to the condylar settings on a semiadjustable articulator. One of the requirements for a stable occlusion is noninterfering posterior teeth. The posterior teeth disclude in eccentric movements due to condylar path, anterior guidance, or a combination of both. Most patients have a minimum condylar path of 25°.7 The normal condylar path setting of a semiadjustable articulator is 20°, flatter than what is normal for most patients. Thus, if posterior teeth are noninterfering on an articulator set at 20°, then they will also be noninterfering in the mouth. In effect, the 20° setting provides a slight margin of error in the dentist’s favor.
The difficulty occurs in the small percentage of patients who present with a condylar path that is flatter than 20°. For them, a protrusive bite record is required and the condylar path on the articulator can be set. The comprehensive examination process will help identify these patients. Then during the records phase, a protrusive bite record can be obtained, aiding in the evaluation and restorative process. Some indicators that a protrusive bite record may be needed are:
- An anterior guidance that does not disclude the posterior teeth. The disclusion is dependant solely on the condylar path.
- Severe wear cases, especially if the maxillary lingual cusps are worn. This indicates a possible flattening of the condylar path.
- Temporomandibular disorders in which complete disk displacement is present or assumed. Without the disk in its proper position, there is an increased risk of flattening the condyle and eminence.
Summary
Face-bow-mounted, centric-relation articulated models on a semiadjustable articulator are key elements to the records process in evaluating and establishing a comprehensive treatment plan, assuring success in the laboratory phase of restorative dentistry. In-office protocols and techniques are required to eliminate as many variables in the process as possible to ensure accuracy. With staff involvement, impeccable mounted models should not take more time to create than it does to generate one with many discrepancies. In fact, a proper set of mounted models is a prerequisite to the treatment planning and restorative phases that will improve accuracy and predictability (Figure 7).
Acknowledgment
The author would like to thank Nancy Barr for her assistance.
References
1. Dawson PE. Functional Occlusion: From TMJ to Smile Design. 1st ed. St. Louis, MO: Mosby;1989:4.
2. Cranham J, Dupont G. Comprehensive Examination and Records. St. Petersburg, FL: The Dawson Academy.
3. Boksman L, Tousignant G. Alginate substitutes: rationale for their use. Dent Today. 2009;28(4):104-105.
4. Dawson PE. Evaluation, Diagnosis and Treatment of Occlusal Problems. 2nd ed. St. Louis, MO: Mosby;1989:238.
5. McKee JR. Comparing condylar position repeatability for standardized versus non-standardized methods of achieving centric relation. J Prosthet Dent. 1997;77(3):280-284.
6. Dawson PE. Functional Occlusion: From TMJ to Smile Design. 1st ed. St. Louis, MO: Mosby;1989:96.
7. Lundeen H, Wirth CG. Condylar movement patterns engraved in plastic blocks. J Prosthet Dent. 1973;30(6): 866-875.
About the Author
Andrew C. Cobb, DDS
Private Practice
Washington, DC