Abstract
Interdental recession or loss of the interdental papilla is one of the greatest challenges facing the dental team. This type of recession defect is due to the loss of the interproximal periodontal attachment apparatus. Treatment planning and its sequencing frequently require not only restorative and periodontal care, but also orthodontic therapy. Orthodontic forced eruption can be one of the most powerful predictable tools and adjunctive techniques in the correction and reconstitution of these vital and delicate tissues.
Many factors must be considered when managing the loss of the interdental papilla on anterior implants in order to determine the best treatment procedure. Loss of the interdental papilla adjacent to a single tooth implant or an edentulous site where implant placement is planned can be considered one of the greatest treatment challenges facing the interdisciplinary dental team. The reason the interdental tissues, or the lack of their presence, is so relevant in clinical dentistry is two-fold: their physical state is usually 4.5 mm more coronal than the midfacial free gingival margin;1-4 and they are present in the esthetic smile 87% to 91% of the time.5,6 Consequently, it is important to understand why these fragile tissues are lost as well as how to render treatment.
Interdental Recession
With the natural dentition, treatment of the loss of the interdental papilla can be complex and unpredictable at best. Even though several authors have offered various surgical treatment solutions, none have been shown to be predictable long term.7,8
Currently, one of the most significant issues in esthetic implant dentistry is malposition of implants. This not only applies to excessive facial angulation and placement,9-11 but also to interproximal.12
One of the major reasons interdental papilla loss occurs on a natural tooth adjacent to a single implant is that the proximal placement is too close, so the horizontal and vertical biologic width formation ultimately compromises the periodontal attachment level on the adjacent tooth.13,14 A second reason for papilla loss would be flap elevation of the interdental papilla upon implant placement; in fact, these authors found that the loss of papilla height could be two to three times greater over a 1-year follow-up period.15
Lastly, the periodontal phenotype—thick versus thin—plays a role in the resistance or susceptibility to interdental recession, respectively.16-19
Treatment
It is the opinion of these authors that the best treatment is avoiding the need for treatment. However, once a patient presents with an interproximal esthetic defect, the outcome of esthetic treatment—which is nonetheless a compromise—can offer a huge improvement.
When treating loss of the interdental papilla, its visual display in the smile is a primary factor to consider.4,5 The papilla must be assessed because its incidence of occurrence in the smile is high.
Treatment options that may be considered by the patient and dental team are: (1) restoration only—ie, using artificial gingiva such as pink ceramics or composite; (2) papillary surgery; and (3) orthodontics. Prosthetic correction may be the most expedient form of correction,20 but it is not accepted by all patients, and surgical correction of the interdental papilla can be highly unpredictable. Orthodontic forced extrusion is the most predictable means of treatment when there is loss of interdental periodontal attachment that is equivalent to the height of the papilla.21-25 Therefore, an orthodontic treatment solution should be considered and implemented, even if there is diminished interproximal attachment remaining on the proximal tooth surface.21
The interproximal attachment level can be moved more coronally with this type of therapy.26 It is not uncommon for elective or prophylactic endodontic therapy to be performed on the treatment tooth prior to orthodontic movement. Considering that the amount of vertical eruption could be greater than 4 mm, it is not unreasonable to expect that the pulp tissues would be compromised after tooth length and occlusion correction.
The restorative dentists should note differences in papillae height before treatment, because one of the goals is alignment of all the interdental papillae in the anterior sextant at the same inciso-gingival level.3
The restorative option should always be discussed with the patient, because it is the first step in treatment and is often the easiest to accomplish. The option to continue further with orthodontic therapy is always available if the patient is not completely satisfied after the provisional restorative phase of treatment. Provisional restoration may involve full or partial coverage with pink acrylic or composite to restoratively replace the missing tissues. This is used to achieve two main objectives: to serve as a visual communication tool to the patient and surgeon to determine how much treatment is needed; and to quantify the amount of orthodontic eruption required. The dental team can then decide the next steps in treatment and sequence with the patient.
Frequently, orthodontic brackets and archwires are used as the mechanical devices. Again, the endpoint of treatment is to achieve equal alignment of all the interdental papillae. Therefore, the tooth in question will be pulled down and the deficient papilla aligned with that of the adjacent teeth. Normally, the midfacial tissues are at the correct height and position prior to treatment, but they will visually appear abnormal relative to the corrected papilla height after orthodontics. In fact, the midfacial tissues relative to the papilla height on the deficient side will appear short. In addition, the papilla on the normal side will be longer if a fiberotomy is not performed during orthodontic therapy.21 In order to reestablish the normal papilla height-to-tooth length ratio of about 40%, midfacial crown lengthening can be performed.
Lastly, orthodontic brackets were not designed with the intent of tooth movement requiring extreme change in vertical position. Consequently, it is not uncommon for the apex of the tooth root to be moved forward and the labial plate of bone to have a facial dehiscence post orthodontic forced eruption. The orthodontist should be aware of this potential occurrence during treatment and be prepared to take counter measures in orthodontic mechanics to avoid this problem, if possible.
As the tooth is moved in a vertical direction, the incisal edge position extrudes with the tooth but is adjusted and removed to a normal position. The crown-to-root ratio is always improved with forced eruption treatment.
Forced eruption can be a 9- to 12-month process—3 to 6 months for eruption and 6 months for stability and retention. If the tooth is not properly retained, it will re-intrude. Papilla-sparing incisions should be followed during implant surgery placement if there is an edentulous site adjacent to the deficient papilla side.
The primary points to remember in treating interdental recession are: first, present the sequential treatment options to the patient with the understanding that orthodontic correction may be the best option to reconstruct the lost native tissues; next, perform forced eruption, which can be a 12-month total process; and then restore the teeth and adjacent implant after healing.
It is imperative to retain the adjacent tooth post-orthodontic treatment. Conceptually, the significance of retaining the adjacent tooth with diminished periodontal support is that it provides supracrestal interproximal biologic width (attachment); if the tooth were extracted, the papilla that was painstakingly regenerated through orthodontic forced eruption would be lost.
Case Report
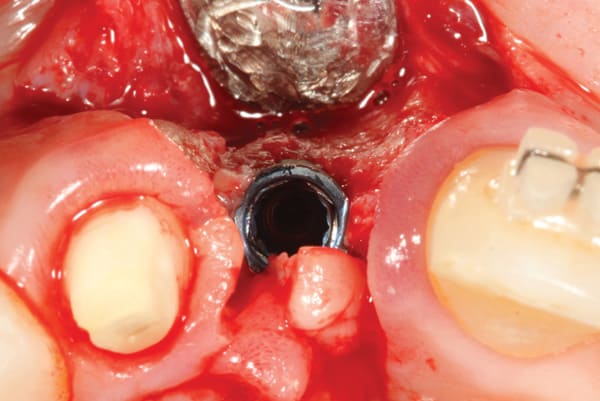
A 38-year old Caucasian female patient presented with a high smile line and loss of the papilla between tooth No. 7 and edentulous adjacent site No. 8 (Figure 1). Understandably, the patient was unhappy and embarrassed about her esthetic condition. Her dental history revealed tooth replacement of No. 8 with an implant that eventually failed. The site had been previously bone grafted upon implant removal. She was given a composite pontic No. 8 bonded to a tooth No. 7 composite veneer as a transitional restoration. The implant was positioned too close to the proximal surface of tooth No. 7, which stripped the periodontal attachment of the root and ultimately caused loss of the papilla (Figure 2). As previously outlined, the treatment sequence would be to first provide a provisional restorative solution to evaluate the projected outcomes and assess if the patient was willing to undergo orthodontic therapy. In this situation, a full-coverage crown No. 7 with a cantilevered pontic No. 8, with artificial acrylic gingiva to replace the lost papilla on the mesial aspect of tooth No. 7 was used as a transitional temporary prosthesis (Figure 3). In addition, a composite resin (Venus® Pearl, Heraeus Kulzer, https://heraeus-kulzer.com) restoration was placed on the mesial aspect of tooth No. 9 to restore its individual tooth proportion and shape. The patient’s esthetic outcome could now be evaluated with restorative correction alone; it was therefore mutually determined that the correction of her deformity would best be served with additional orthodontic forced eruption therapy. A fixed orthodontic appliance (brackets) was bonded to the teeth and temporary prosthesis. The level of the interproximal pink acrylic was used as a therapeutic guide for the amount of forced eruption required as well as the alignment of the mesial papilla of No. 7 to that of the adjacent papillae height (Figure 4). Floss was used to elevate the amount of vertical movement achieved relative to the adjacent papilla tooth No. 9. Eventually, all the artificial pink acrylic was removed. (Note that the distal papilla on tooth No. 7 also comes more incisal—in fact, it is slightly excessive at the endpoint of treatment [Figure 5]). However, the distal papilla and midfacial tissues of tooth No. 7 can be reshaped through clinical crown lengthening toward the end of treatment prior to definitive restoration, thereby restoring the proper papilla height-to-tooth ratio of 40%. After stabilization of tooth No. 7 for a minimum of 6 months post-orthodontics, an implant was placed in site No. 8. A papilla-sparing incision design was used for flap elevation (Figure 6), bone allograft (Puros® Demineralized Bone Matrix, Zimmer, www.zimmer.com) was used to further augment the facial aspect of the ridge simultaneously with implant placement (Certain® Implant System, Biomet 3i, www.biomet3i.com) (Figure 7), and a resorbable membrane (BioMendExtend, Zimmer) was used for guided bone regeneration.
After 6 months of healing of the implant, stage 2 uncovering was performed and the mucosal tissues were allowed to mature for another 2 to 3 weeks. A temporary screw-retained implant cylinder (PreFormance® Temporary Cylinder, Biomet 3i) was joined to the implant and acrylic (Super-T, American Consolidated Mfg, www.pattersondental.com) crown (Figure 8). The subgingival shape of the temporary was modified with additional acrylic and the technique of non-surgical tissue sculpting, which was developed to provide the proper emergence profile to the mucosal tissues.27 It is important that the temporary blanching (ischemia) of the mucosal tissues dissipate after 10 minutes (Figure 9). After 3 weeks, soft-tissue scalloping through gingivectomy was done to recreate the proper shape (ie, gingival zenith)28 and proportion for the mucosal tissues (Figure 10). Fiberotomy on the distal aspect of tooth No. 7 was not performed during treatment; therefore, this papilla was slightly more incisal (longer) than the adjacent papillae (Figure 11). A final impression was made of crown No. 7 and implant No. 8 at the implant level to enable a working cast to be made in the laboratory. An all-ceramic custom abutment was made for implant No. 8 (BellaTek® Encode, Biomet 3i), and splinted full-coverage units were made for crowns No. 7 and No. 829 (Figure 12). The custom abutment was seated intraorally and torqued according to the manufacturer’s recommendation. The crowns were luted with provisional cement (Tempbond® NE, Kerr Dental, www.kerrdental.com) and maintained at 4-month recall intervals (Figure 13). Note the health of the periodontal tissues and their integration with the adjacent teeth and surrounding gingiva, taking a complex esthetic and functional problem for a patient with a high smile line and providing a predictable restorative and esthetic outcome (Figure 14).
Conclusion
Treatment of the loss of the interdental tissues can be a complex and compromised endeavor requiring orthodontic, periodontal, and restorative care. Orthodontic forced eruption may be the most predictable treatment option to reconstruct these violated tissues.
It is important to remember the following key clinical elements: (1) use the temporary restoration with artificial gingiva to visualize the treatment outcome; (2) stabilize the tooth for at least 6 months post-orthodontic movement; (3) retain the affected tooth after vertical position correction, because it offers supracrestal biologic width (periodontal attachment); and (4) join the tooth to the implant as a splinted unit when using full-coverage restorations.
Proper treatment planning and sequencing are critical for a predictable and lasting biologic and esthetic outcome.
References
1. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
2. Kois, JC. Altering gingival levels: The restorative connection. Part I: Biologic variables. J Esthet Dent. 1994;6:3-9.
3. Spear, FM. Maintenance of the interdental papilla following anterior tooth removal. Pract Periodont Aesthet Dent. 1999;11(1):21-28.
4. Chu SJ, Tarnow DP, Tan J H, Stappert, C. Papilla proportions in the maxillary anterior dentition. Int J Periodontics Restorative Dent. 2009;29(4):385-393.
5. Tjan AH, Miller GD, The JG. Some esthetic factors in a smile. J Prosthet Dent. 1984;51(1):24-28.
6. Hochman MN, Chu SJ, Tarnow DP. Maxillary anterior papillae display during smiling: A clinical study of the interdental smile line. Int J Periodontics Restorative Dent. 2012;32(4):375–383.
7. Prato GP, Rotundo R, Cortellini P et al. Interdental papilla management: A review and classification of the therapeutic approaches. Int J Periodont Rest Dent. 2004;24(3):246-255.
8. Nordland WP, Sandhu HS, Perio C. Microsurgical technique for augmentation of the interdental papilla: Three case reports. Int J Periodont Rest Dent. 2008;28(6):543-549.
9. Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin Oral Implants Res. 2007;18(5):552–562.
10. Evans CD, Chen ST. Esthetic outcomes of immediate implant placement. Clin Oral Implants Res. 2008;19(1):73-80.
11. Cooper LF, Raes F, Reside GJ, et al. Comparison of radiographic and clinical outcomes following immediate provisionalization of single-tooth dental implants placed in healed alveolar ridges and extraction sockets. Int J Oral Maxillofac Implants. 2010;25(6):1222-1232.
12. Esposito M, Ekestubbe A, Grondahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single branemark implants. Clin Oral Implants Res. 1993;4(3):151-157.
13. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of the inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
14. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75(9):1242-1246.
15. Gomez-Roman G. Influence of flap design on peri-implant interproximal crestal bone loss around single-tooth implants. Int J Oral Maxillofac Implants. 2001;16(1):61–67.
16. Olsson M, Lindhe J. Periodontal characteristics in individuals with varying forms of the upper central incisors. J Clin Periodontol. 1991; 18: 78-82.
17. Kan JY, Rungcharassaeng K, Umezu K, Kois JC.. Dimensions of peri-implant mucosa: An evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74(4):557-562.
18. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-219.
19. Linkevicius T, Apse P, Grybauskas S, Puisys A. Reaction of crestal bone around implants depending on mucosal tissue thickness. A 1 year prospective clinical study. Stomatologija. 2009;11(3):83-91.
20. Coachman C, Salama M, Garber D, et al. Prosthetic gingival reconstruction in a fixed partial restoration. Part 1: introduction to artificial gingiva as an alternative therapy. Int J Periodontics Restorative Dent. 2009;29(5):471-477.
21. Pontoriero R, Celenza F Jr, Ricci G, Carnevale G. Rapid extrusion with fiber resection: A combined orthodontic-periodontic treatment modality. Int J Periodontics Restorative Dent. 1987;7(5):30-43.
22. Ingber IS. Forced eruption: Part I. J Periodontol. 1974;45:199–206.
23. Ingber IS. Forced eruption: part II. A method of treating nonrestorable teeth—Periodontal and restorative considerations. J Periodontol. 1976;47(4):203–216.
24. Ingber JS. Forced eruption: alteration of soft tissue cosmetic deformities. Int J Periodontics Restorative Dent. 1989;9(6):416–425.
25. Salama, H, Salama, M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction defects. Int J Periodont Rest Dent. 1993;13(4):313-333.
26. Amato F, Mirabella AD, Macca U, Tarnow DP. Implant site development by orthodontic forced extraction: A preliminary study. Int J Oral Maxillofac Implants. 2012;27(2):411-420.
27. Zamzok, J. Avoiding ridge laps through nonsurgical soft tissue sculpting on implant restorations. J Esthet Rest Dent. 1996;8(5):222-228.
28. Chu SJ, Tan JH, Stappert CF, Tarnow DP. Gingival zenith positions and levels of the maxillary anterior dentition. J Esthet Restor Dent. 2009;21(2):115–123.
29. Lindh T. Should we extract teeth to avoid tooth-implant combinations? J Oral Rehabilitation. 2008;35 Supple 1:44-54.
About the Authors
Stephen J. Chu, DMD, MSD, CDT
Clinical Associate Professor Director of Esthetic Education, Columbia University College of Dental Medicine
New York, NY
Mark N. Hochman, DDS
Private Practice,
New York, NY
Dennis P. Tarnow, DDS
Clinical Professor, Director of Implant Education Columbia University College of Dental Medicine
New York, NY