It is estimated that more than 32 million people in the United States are edentulous, and 12 million new dentures are made annually. The 65+ age group will double by 2030, making it the fastest-growing age group in the United States. Additionally, the partially edentulous population will increase to 200 million people.1-3 Among existing dentures, some 75% are due for replacement, according to their 7-year life cycle.
Unfortunately, despite the obvious need and growing demand for removable dental prosthetics, traditional processes used to create them are time-consuming and problematic for dentists and patients alike.4 The usual first patient visit for dentures involves taking a preliminary impression, which is then forwarded to the laboratory to create a custom tray. This is returned to the dentist for the second patient visit, during which the dentist takes a final impression. This impression is returned to the dental laboratory, where a base plate and occlusal rims are made.
After the base plate and occlusal rims are returned to the dentist, a third patient visit is scheduled to determine the vertical dimension and centric relation. Once established, this information is forwarded to the laboratory for production of an analog wax-up for try-in. At the fourth patient visit, the dentist evaluates the try-in in the patient’s mouth, and it is returned to the laboratory for processing and finishing of this analog denture. It is finally at the fifth patient appointment that the dentist can deliver and fit the final denture. Any necessary adjustments are then completed at the sixth and any subsequent visit(s).
An Efficient Digital Denture Process
Digital dentures created with new technology based on CAD/CAM and 3D printing (Pala Dentures, Heraeus Kulzer, www.heraeus-kulzer-us.com) eliminate this time-consuming process, one that is wrought with numerous challenges and inaccuracies (eg, poor fit, porous composition prone to staining and odor, improper occlusal schemes, unesthetic tooth shape or arrangement).5,6
With digital 3D printing dentures, all of the information needed to design the denture is captured in one dental office visit and stored in digital format. The digital process allows for fabrication of an extremely precise and accurate denture, and denture teeth from a number of sources can be used. The process requires fewer patient dental office visits—two or three—and the patient spends less time—under 45 minutes—in the dental chair. It is not as labor intensive or as costly as traditional dentures. Digital data can be retained for future use, which allows for fabrication of a spare or replacement denture or modification of a previous denture, if needed.7
Pala Digital Dentures are suitable for single- and full-arch cases and implant overdentures. Dentists need only take impressions with Pala trays, as indicated in the impression manual, and provide the required records (ie, upper and lower impressions, bite, centric relation and vertical dimension, and photograph of patient’s midline, if possible).
The following case presentation demonstrates the manner in which full-arch Pala Digital Dentures were planned, tried-in, and fabricated with only one patient appointment after tooth extraction. The mandibular Pala Digital Denture, in particular, was finalized in only three appointments, and it was ready for immediate retrofitting and loading on the day of implant placement.
Case Presentation
A female patient employed at a convenience store located near the author’s practice presented with severely broken down and decayed teeth (Figure 1 and Figure 2). In expressing a desire for help, she said that since her husband’s death, she had neglected herself and, due to visibly extensive dental disease, refrained from smiling.
A comprehensive examination and complete diagnostic work-up that included digital radiographs, photographs, and a periodontal evaluation were completed. It was determined that all teeth required extraction, and that immediate dentures would be provided (Figure 3). Subsequent treatment would involve placing four implants in the mandible to support a final digital denture, as well as a digital denture for the maxillary arch.8
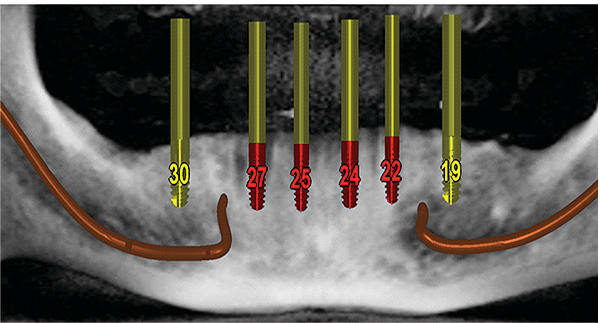
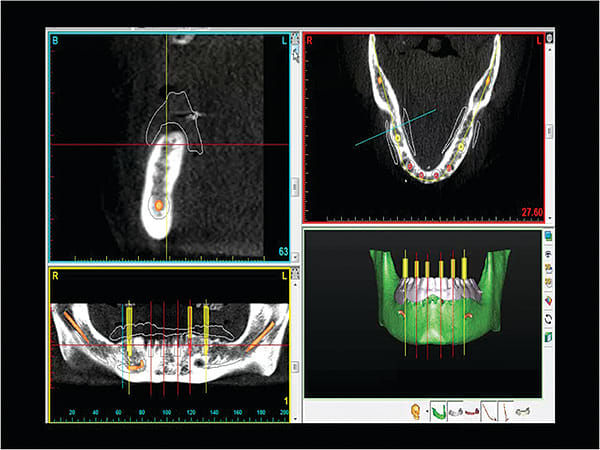
After healing, a CBCT scan was taken to assess the patient’s bone, plan implant placement (Figure 4 and Figure 5), and facilitate implant surgical guide fabrication (Figure 6 and Figure 7).9,10 The patient exhibited good bone, which would facilitate implant placement and retrofitting a digital mandibular removable prosthesis into an immediately loaded implant-retained overdenture.11
Prior to implant placement, steps were undertaken to produce the final digital dentures.
Digital Denture Impression-Taking (First Appointment)
To fabricate the digital denture (Pala Denture), a preliminary impression was taken using special trays specifically for creating digital impressions of the oral cavity (Pala Digital Denture Trays). The correct tray size that best fit the patient’s mouth (ie, slightly larger) was selected by trying directly in the patient’s mouth (Figure 8). First, the maxillary tray was completely filled with fast-setting, high-density PVS material, taking care to cover the entire tray surface with sufficient material. The tray was gently seated all the way in the patient’s mouth and held firmly upward by pressing up on the center and two finger spots on each side of the tray (Figure 9). The patient was instructed to relax her mouth and move her jaw side to side, after which her cheeks were stretched out, one at a time. This was essential for capturing the smooth contours where the denture’s borders would meet the soft tissue.
The tray was removed, and a light-body wash material about 1-mm to 2-mm thick was placed to cover the entire tray and impression area to capture all muscle details of the patient’s mouth. The tray was re-seated firmly into the patient’s mouth and held in place. The patient was instructed to relax her muscles during border molding movements. The tray was removed, and the same steps were followed to obtain the mandibular impression.
The impression trays were then used to record bite dimensions, as well as the vertical dimensions of occlusion (VDO) and centric relation (CR). A screw pin was attached to the mandibular tray in the highest position, after which the maxillary tray was firmly seated in the patient’s mouth. The mandibular tray with the pin pointed toward the top was then gently placed in the patient’s mouth, and the patient was instructed to close gently and not bite too hard. With the mandibular tray firmly seated in the mouth, VDO was adjusted by rotating the center pin clockwise to lower the height.
After arriving at the correct VDO with the patient’s lips barely touching, the CR was traced at this vertical dimension using the center pin as a gothic arch tracer. A small amount of tracing material was applied on the lower side of the maxillary tray, and the patient was instructed to move her jaw in and out and side by side to trace the gothic arch.
The tray was removed and a small hole was drilled at the apex to mark the CR, which was where the lower pin was locked when taking the bite registration. Once the trays were locked into position, bite registration material was injected into the space between the trays to capture the VDO and CR simultaneously (Figure 10).
Finally, the lip length (ie, smile line) was measured (Figure 11). The impressions and records obtained during this first appointment were sent to the dental laboratory for creating the digital denture try-in.
Laboratory Protocol
At the laboratory, the impressions and bite records were converted into a computer-generated impression using a 3D scanner (3Shape), after which they were digitally articulated to the bite—open and closed—using automatic impression recognition. Teeth were digitally placed according to the optimal teeth arch shape, shade, and measurements provided by the dentist. In particular, the software contextualized 26 anatomical landmarks in the impression to generate the midline, occlusal plane, Curve of Spee, and Curve of Wilson, among other aspects. Then, the files and prescription information were sent to the Pala Denture Center, where the denture models were loaded into the 3D printer (Objet, Stratasys, www.stratasys.com) to create the 3D printed try-in prototype.
Digital Denture Try-in (Second Appointment)
The 3D printed prototype was shipped to the dentist for try-in. The try-in dentures were placed in the mouth and closely evaluated to ensure all previous measurements, information, and adjustments were replicated. At this appointment, functional aspects (eg, retention, fit, midline, occlusion, vertical dimension, phonetics, chewing) were evaluated. Additionally, esthetic considerations (eg, smile line, lip support, setup) were also examined.
In this case, the patient exhibited too much of a gummy smile. As a result, the 3D prototype was marked with changes for correcting this esthetic aspect (Figure 12), and was then returned for processing. The Pala Digital Denture certified modeler finalized the denture model and made necessary adjustments. The virtual denture was then finalized using a proprietary injection process to convert the 3D-printed try-in to the final denture, which was forwarded back to the dentist (Figure 13).
Implant Placement & Digital Denture Retro-fitting (Third Appointment)
The final prosthesis was tried in, confirming it could be immediately retrofitted and loaded on the day of implant surgery. The four implants were placed using a surgical guide (Figure 14), and the digital denture was retrofitted and seated at that time (Figure 15).12
Conclusion
The ability to perform a virtual wax-up by setting and moving the denture teeth on a computer, and then using the 3D prototype for try-in, contributes to efficiency and accuracy. Instead of using wax rims and plates that sometimes do not sit well, the 3D prototypes/try-ins provide a better representation of how the proposed dentures will look, fit, and function.
In the traditional wax-rim process, the master cast and master impression are poured for making a base plate that is molded to the impression. The wax rim is placed on top for support, but it doesn’t fit or feel like the final prosthesis will. Because the prototype represents the actual way the final denture will fit, the try-in process with digital dentures is much easier, less time consuming, and contributes to a greater accuracy.
In the case presented, Pala Digital Dentures provided a cost-effective and efficient denture solution by eliminating appointments, thereby shortening denture-related treatment and chairtime. No investment in any 3D CAD/CAM hardware or software was required by the practice, and the process involved significantly fewer steps than traditional denture procedures, but with greater accuracy. The patient really only needed to come into the practice for two or three visits before obtaining her final denture, which significantly improved her oral function and greatly enhanced her appearance (Figure 16 and Figure 17).
About the authors
David Little, DDS
Private Practice
Professionals in Dentistry
San Antonio, Texas
Kristen McBride, DDS
Private Practice
Professionals in Dentistry
San Antonio, Texas
References
1. National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD. 2012.
2. U.S. Census Bureau. U.S. Interim Projections By Age, Sex, Race, and Hispanic Origin: 2000–2050. Suitland, MD: U.S. Census Bureau Population Division; 2004.
3. Douglass CW, Shih A, Ostry L. Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 2002;87(1):5-8.
4. Rudd RW, Rudd KD. A review of 243 errors possible during the fabrication of a removable partial denture: part I. J Prosthet Dent. 2001;86(3):251-261.
5. Li W, Yuan F, Lv P, Wang Y, Sun Y. Evaluation of the quantitative accuracy of 3D reconstruction of edentulous jaw models with jaw relation based on reference point system alignment. PMC Biophys. 2015;10(2):e0117320.
6. Infante L, Yilmaz B, McGlumphy E, Finger I. Fabricating complete dentures with CAD/CAM technology. J Prosthet Dent. 2014;111(5):351-355.
7. Bidra AS, Taylor TD, Agar JR. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives. J Prosthet Dent. 2013;109(6):361-366.
8. Little DA, Buckley SB, Saunders R. Providing stable and esthetic screw-retained implant dentures with minimal patient visits. Inside Dental Technology. 2012;3(Spec Iss 1):1-3.
9. Rossi R, Morales RS, Frascaria M, Benzi R, Squadrito N. Planning implants in the esthetic zone using a new implant 3D navigation system. Eur J Esthet Dent. 2010;5(2):172-188.
10. Orentlicher G, Horowitz A, Abboud M. Guided implant surgery: indications and guidelines for use. Compend Cont Educ Dent. 2012;30(10):720-732.
11. Lozada JL, Garbacea A, Goodacre CJ, Kattadiyil MT. Use of a digitally planned and fabricated mandibular complete denture for easy conversion to an immediately loaded provisional fixed complete denture. Part 1. Planning and surgical phase. Int J Prosthodont. 2014;27(5):417-421.
12. Agliardi E, Panigatti S, Clerico M, Villa C, Malo P. Immediate rehabilitation of the edentulous jaws with full fixed prostheses supported by four implants: interim results of a single cohort prospective study. Clin Oral Implants Res. 2010;12(5):459-465.